The umbrella term NIPPV includes modes in which - in addition to CPAP/PEEP - controlled breaths are applied to support the patient. These breaths have a higher pressure level and are not emitted in a synchronized manner. A differentiation is made between the different variants of this form of respiratory support (
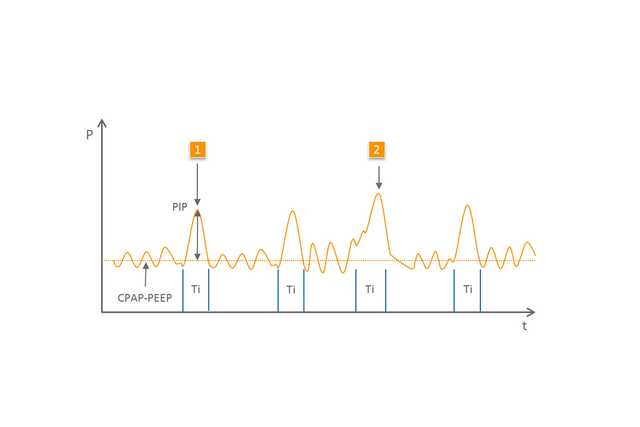
NIPPV (
Controlled respiratory support for neonates
Effective support after extubation and during apnea (1,2)
Easy to use and adjust
Available in the medinCNO, medinCNOmini, medin-NC3 devices
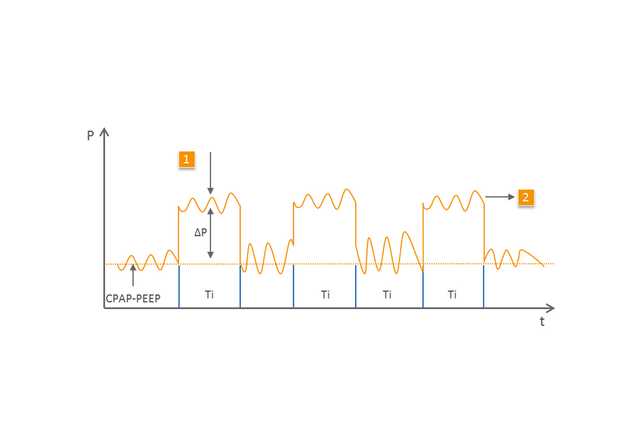
The BiLevel (
1 Mechanical breath
2 Spontaneous breathing on the second, higher pressure level
The effects and efficacy of NIPPV were investigated in numerous studies (
The specialized CPAP devices from medin in connection with the Medijet nCPAP generator are ideally suited for the use of NIPPV and BiLevel. With basic flow, the patient is provided with the desired CPAP/PEEP. With the aid of a second flow level which is set in addition to the basic flow via an additional electronic flow meter, Medijet generates a higher pressure level.
Since Medijet allows expiration at any point in time, the patient can breathe freely at both pressure levels. Because of this, the medin CPAP devices allow all NIPPV respiratory support options.