SNIPPV is the synchronized variant of the NIPPV respiratory support. In NIPPV, the breaths are administered by the device independent of the patient’s own breathing. This can lead to conflicts in the synchronization between the patient and the device. In SNIPPV, the breaths are coordinated to the patient’s inspiration and conflicts are minimized.
Studies were not only able to demonstrate the efficacy of SNIPPV. SNIPPV is superior in many indications compared to conventional modes such as nCPAP and NIPPV: (
Effective synchronized support
MediTRIG technology without an additional sensor
Apnea treatment (and backup frequency)
Available in the medinCNO device
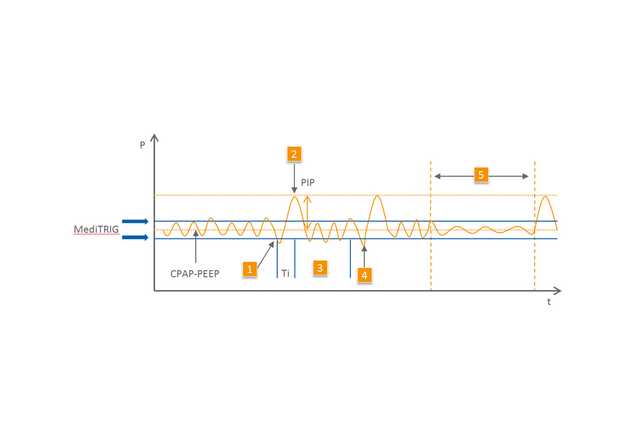
The type of trigger system plays an important role. The innovative pressure trigger system MediTRIG detects the patient’s airway pressures and from them, it can identify the start of inspiration. The spontaneous breaths are supported by breaths from the device with additional pressure.
MediTRIG does not require any additional sensor to record the patient’s own breathing, such as in the case of an abdominal capsule. MediTRIG gently detects the necessary signals directly at the nose of the small patient.
The apnea functions are also available in SNIPPV mode. The SNIPPV and MediTRIG parameters can be individually adapted to the patient.
SNIPPV is defined by inspiration times which are as short as possible (0.2-0.5 sec) and breath rates up to 90/100 BPM. SNIPPV is a time-controlled mode, that is, the breath frequency is first and foremost set via the inspiration time and an expiration pause. In the expiration pause, the patient breathes on the CPAP level and the device does not emit any supportive breaths. In this way, the support can be individually adapted to the patient's needs. The level of pressure support is individually coordinated to the patient's needs with the aid of a second flow level.