

Apnea and breathing irregularities affect nearly every premature infant and newborn. The more premature the infant is, the more markedly apnea occurs. They represent a disruption in the respiratory mechanics as well as respiratory control. The most important feature of the apnea is the intermittent air flow in the patient’s airway.
Apnea is clinically significant for the patient due to the concomitant symptoms such as bradycardia <80 BPM (decreased heart rate) and hypoxia <80% (decreased oxygen saturation). The goal of prophylaxis and treatment of apnea is to avoid or minimize negative effects (
Additional breaths stimulate respiration
Airways are stabilized which facilitates breathing as a result
The patient’s own breathing is detected and the device switches into CPAP mode
Available in the devices medinCNO, medinCNOmini, medin-NC3
The efficacy of nasal CPAP is proven in this context by studies and is a part of the applicable guidelines for the treatment of apnea and its concomitant symptoms (
The mechanisms of action are:
The medin ApneaCPAP with apnea treatment can be used from the prophylaxis to the treatment of existing apnea.
Based on the nCPAP mode, central and obstructive apnea is detected with the unique MediTRIG technology and responded to with automatic additional breaths from the CPAP device. The level of the peak pressure of the breaths is adjusted with a second electronic flow meter and added to the basic flow. The parameters of the ApneaCPAP function as well as of the MediTRIG can be individually adapted to the patient.
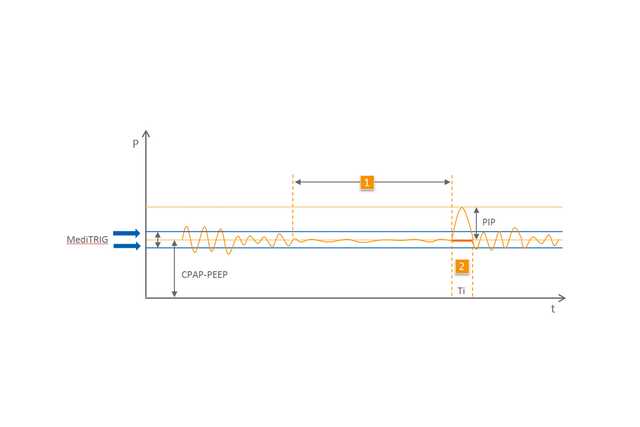
1 Apnea
2 Automated breath