

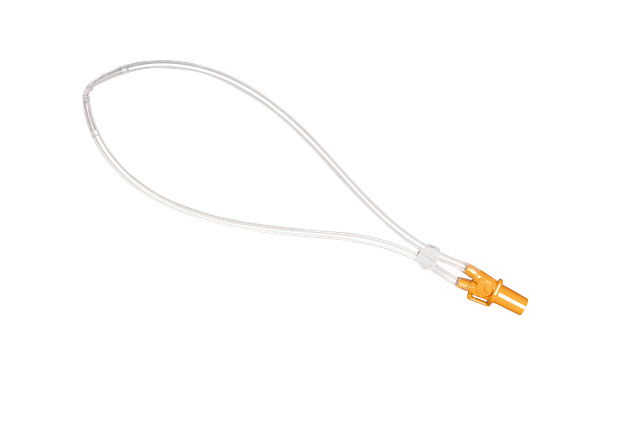
La cánula nasal de flujo alto Nuflow de medin está fabricada con una silicona suave diseñada para el cuidado de la piel que ofrece el equilibrio perfecto entre comodidad y eficacia de la terapia. Incluso el tamaño de cánula más pequeño proporciona magnitudes de flujo de hasta 8 l/min y, por lo tanto, cumple las directrices actuales de aplicación de la terapia con flujo alto de oxígeno para neonatología (
Se pueden utilizar otros tamaños de cánula para bebés y recién nacidos en combinación con un respirador adecuado, por ejemplo, de Hamilton Medical.
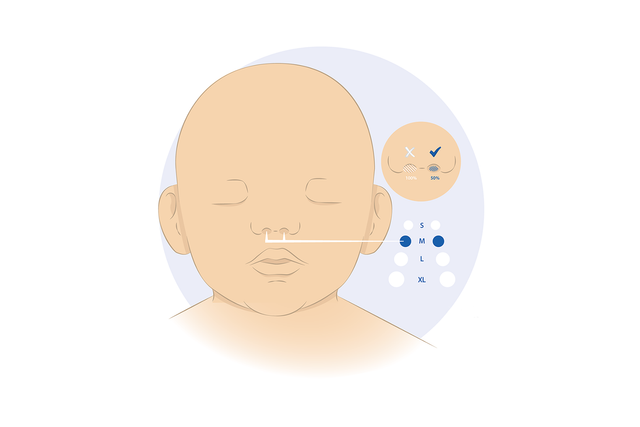
Al menos el 50 % de la fosa nasal queda despejada para: