

La nCPAP (presión nasal positiva continua en la vía aérea) es el modo de soporte respiratorio no invasivo utilizado con más frecuencia en bebés prematuros y recién nacidos, así como la base para otras variantes, como la ventilación nasal con presión positiva intermitente (NIPPV), la ventilación nasal con presión positiva intermitente sincronizada (SNIPPV) y la ventilación nasal de alta frecuencia (nHFV). Al utilizar la nCPAP, el paciente debe ser capaz de respirar espontáneamente, dado que esta terapia no administra respiraciones adicionales.
El parámetro más importante de la terapia nCPAP es la PEEP, que corresponde a la presión positiva en la vía aérea al final de la espiración (por sus siglas en inglés).
Durante la respiración espontánea sin nCPAP, las presiones inspiratorias pueden alcanzar en ciertos casos valores negativos en las vías aéreas. La nCPAP permite mantener el ciclo respiratorio completo del paciente, incluidas inspiración y espiración, en niveles de presión positiva.
Mejora de la oxigenación
Prevención del colapso alveolar
Reducción del esfuerzo respiratorio
Mantenimiento de la capacidad funcional residual
Estabilización de las vías aéreas (
medinCNO, medinCNOmini y medin-NC3 ofrecen la función nCPAP junto con modos de ventilación ampliados, como ApneaCPAP, NIPPV, SNIPPV o nHFV. El mezclador EasyBlender, el sistema BubbleCPAP y el dispositivo medinSINDI solo funcionan con el modo nCPAP.
Además de estos dispositivos nCPAP específicos, también se pueden utilizar diversos respiradores, por ejemplo, los dispositivos de Hamilton Medical.
Todas estas variantes comparten una característica, que es su capacidad para generar presión en las vías aéreas del paciente mediante la interacción del flujo de gas respiratorio y las resistencias definidas. El tipo de interfaz nasal desempeña una función muy importante en este sentido.

La interfaz nCPAP (Miniflow) se puede conectar a un respirador, una unidad de control o un sistema BubbleCPAP a través de una rampa inspiratoria y espiratoria del sistema de tubos.
Al final de la rama espiratoria, hay una válvula que se abre o se cierra en función de la PEEP seleccionada. El flujo de gas que circula en el sistema crea la presión deseada en esta válvula.

Las interfaces nasales de estos sistemas (Medijet) están equipadas con una válvula que genera la presión directamente en la interfaz, junto con el flujo de gas. Por este motivo, también reciben el nombre de generadores de CPAP.
Es habitual utilizar un sistema de tubos con una única rama inspiratoria en combinación con un dispositivo CPAP.
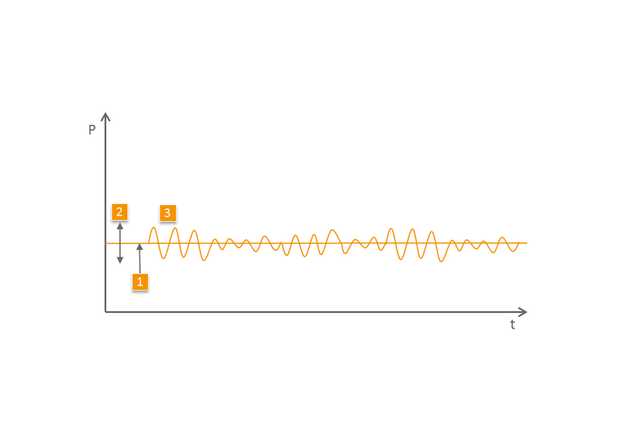
1 PEEP/CPAP
2 Amplitud de la respiración espontánea con respecto a la PEEP
3 Señal de presión de respiración espontánea