La SNIPPV es la variante sincronizada del soporte respiratorio con NIPPV. En la NIPPV, el dispositivo administra las respiraciones independientemente de la propia respiración del paciente. Esto puede provocar conflictos de sincronización entre el paciente y el dispositivo. En la SNIPPV, las respiraciones se coordinan con la inspiración del paciente y, de este modo, la incidencia de conflictos se reduce al mínimo.
Los estudios, no solo han demostrado la eficacia de la SNIPPV, sino también que ofrece mejores resultados que los modos convencionales, como la nCPAP y la NIPPV, en diversas indicaciones: (
Soporte sincronizado eficaz
Tecnología MediTRIG sin un sensor adicional
Tratamiento de la apnea (y frecuencia de respaldo)
Disponible en el dispositivo medinCNO
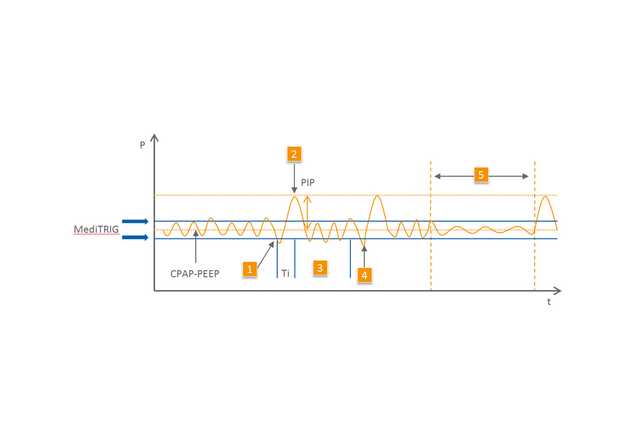
El tipo de sistema de disparo desempeña una función muy importante. El innovador sistema de disparo por presión MediTRIG detecta los niveles de presión en la vía aérea del paciente y, a partir de estas, es capaz de identificar el inicio de la inspiración. Las respiraciones espontáneas están asistidas por las respiraciones generadas por el dispositivo, que aplican una presión adicional.
MediTRIG no requiere ningún sensor adicional para registrar las respiraciones del paciente, como sucede con una cápsula abdominal. MediTRIG detecta suavemente las señales necesarias en la nariz del pequeño paciente.
Las funciones de detección de apnea también están disponibles en el modo SNIPPV. Los parámetros de SNIPPV y MediTRIG se pueden adaptar a cada paciente de forma individual.
El modo SNIPPV se caracteriza por tiempos de inspiración con una duración mínima (0,2 a 0,5 s) y frecuencias respiratorias de hasta 90/100 l/min. En el modo SNIPPV, el tiempo es un parámetro primordial, lo que implica que la frecuencia respiratoria depende fundamentalmente del tiempo inspiratorio y la pausa espiratoria definidos. En la pausa espiratoria, el paciente respira en el nivel de CPAP y el dispositivo no genera ninguna respiración de soporte. Esto permite adaptar el soporte a las necesidades individuales de cada paciente. El nivel de la presión de soporte se coordina con las necesidades individuales de cada paciente con la ayuda de un segundo nivel de flujo.